Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
- Impact of Post-Transplant Diabetes Mellitus on Survival and Cardiovascular Events in Kidney Transplant Recipients
- Ja Young Jeon, Shin Han-Bit, Bum Hee Park, Nami Lee, Hae Jin Kim, Dae Jung Kim, Kwan-Woo Lee, Seung Jin Han
- Endocrinol Metab. 2023;38(1):139-145. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1594
- 1,660 View
- 120 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
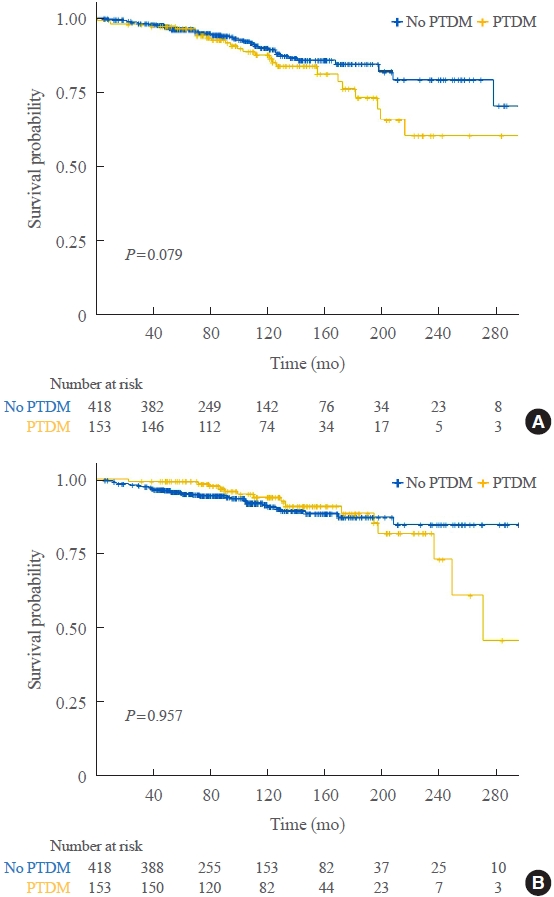
Post-transplant diabetes mellitus (PTDM) is a risk factor for poor outcomes after kidney transplantation (KT). However, the outcomes of KT have improved recently. Therefore, we investigated whether PTDM is still a risk factor for mortality, major atherosclerotic cardiovascular events (MACEs), and graft failure in KT recipients.
Methods
We studied a retrospective cohort of KT recipients (between 1994 and 2017) at a single tertiary center, and compared the rates of death, MACEs, overall graft failure, and death-censored graft failure after KT between patients with and without PTDM using Kaplan-Meier analysis and a Cox proportional hazard model.
Results
Of 571 KT recipients, 153 (26.8%) were diagnosed with PTDM. The mean follow-up duration was 9.6 years. In the Kaplan- Meier analysis, the PTDM group did not have a significantly increased risk of death or four-point MACE compared with the non-diabetes mellitus group (log-rank test, P=0.957 and P=0.079, respectively). Multivariate Cox proportional hazard models showed that PTDM did not have a negative impact on death or four-point MACE (P=0.137 and P=0.181, respectively). In addition, PTDM was not significantly associated with overall or death-censored graft failure. However, patients with a long duration of PTDM had a higher incidence of four-point MACE.
Conclusion
Patient survival and MACEs were comparable between groups with and without PTDM. However, PTDM patients with long duration diabetes were at higher risk of cardiovascular disease. -
Citations
Citations to this article as recorded by- Effect of post-transplant diabetes mellitus on cardiovascular events and mortality: a single‐center retrospective cohort study
Uğur Ünlütürk, Tolga Yıldırım, Merve Savaş, Seda Hanife Oğuz, Büşra Fırlatan, Deniz Yüce, Nesrin Damla Karakaplan, Cemile Selimova, Rahmi Yılmaz, Yunus Erdem, Miyase Bayraktar
Endocrine.2024;[Epub] CrossRef - Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Safety and efficacy of semaglutide in post kidney transplant patients with type 2 diabetes or Post-Transplant diabetes
Moeber Mohammed Mahzari, Omar Buraykan Alluhayyan, Mahdi Hamad Almutairi, Mohammed Abdullah Bayounis, Yazeed Hasan Alrayani, Amir A. Omair, Awad Saad Alshahrani
Journal of Clinical & Translational Endocrinology.2024; 36: 100343. CrossRef
- Effect of post-transplant diabetes mellitus on cardiovascular events and mortality: a single‐center retrospective cohort study

- Clinical Guidelines for the Management of Adrenal Incidentaloma
- Jung-Min Lee, Mee Kyoung Kim, Seung-Hyun Ko, Jung-Min Koh, Bo-Yeon Kim, Sang Wan Kim, Soo-Kyung Kim, Hae Jin Kim, Ohk-Hyun Ryu, Juri Park, Jung Soo Lim, Seong Yeon Kim, Young Kee Shong, Soon Jib Yoo
- Endocrinol Metab. 2017;32(2):200-218. Published online June 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.200
- 16,201 View
- 690 Download
- 80 Web of Science
- 78 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader An adrenal incidentaloma is an adrenal mass found in an imaging study performed for other reasons unrelated to adrenal disease and often accompanied by obesity, diabetes, or hypertension. The prevalence and incidence of adrenal incidentaloma increase with age and are also expected to rise due to the rapid development of imaging technology and frequent imaging studies. The Korean Endocrine Society is promoting an appropriate practice guideline to meet the rising incidence of adrenal incidentaloma, in cooperation with the Korean Adrenal Gland and Endocrine Hypertension Study Group. In this paper, we discuss important core issues in managing the patients with adrenal incidentaloma. After evaluating core proposition, we propose the most critical 20 recommendations from the initially organized 47 recommendations by Delphi technique.
-
Citations
Citations to this article as recorded by- The improvement of postoperative blood pressure and associated factors in patients with hormone‐negative adrenal adenoma and hypertension
Jiaxing Sun, Yingchun Dong, Hanbo Wang, Xudong Guo, Ning Suo, Shangjian Li, Xiangbin Ren, Shaobo Jiang
Journal of Surgical Oncology.2024; 129(6): 1073. CrossRef - Clinical features and treatment options for pediatric adrenal incidentalomas: a retrospective single center study
Xiaojiang Zhu, Saisai Liu, Yimin Yuan, Nannan Gu, Jintong Sha, Yunfei Guo, Yongji Deng
BMC Pediatrics.2024;[Epub] CrossRef - Characterizing incidental mass lesions in abdominal dual-energy CT compared to conventional contrast-enhanced CT
Jack Junchi Xu, Peter Sommer Ulriksen, Camilla Wium Bjerrum, Michael Patrick Achiam, Timothy Andrew Resch, Lars Lönn, Kristoffer Lindskov Hansen
Acta Radiologica.2023; 64(3): 945. CrossRef - Metastatic Adrenal PEComa: Case Report and Short Review of the Literature
Enrico Battistella, Luca Pomba, Marica Mirabella, Michele Gregianin, Antonio Scapinello, Marco Volante, Antonio Toniato
Medicina.2023; 59(1): 149. CrossRef - Surgical management and outcomes of spinal metastasis of malignant adrenal tumor: A retrospective study of six cases and literature review
Xiangzhi Ni, Jing Wang, Jiashi Cao, Kun Zhang, Shuming Hou, Xing Huang, Yuanjin Song, Xin Gao, Jianru Xiao, Tielong Liu
Frontiers in Oncology.2023;[Epub] CrossRef - An adrenal incidentaloma that had appeared to produce dehydroepiandrosterone-sulfate in excess before immunohistochemical study of the tumor
Toshihide Yamamoto, Takuma Kimura, Yuki Kubo, Shin-ichi Nakatsuka, Hiromasa Harada, Takashi Suzuki, Hironobu Sasano
Endocrine Journal.2023; 70(1): 43. CrossRef - Mortality Not Increased in Patients With Nonfunctional Adrenal Adenomas: A Matched Cohort Study
Albin Kjellbom, Ola Lindgren, Malin Danielsson, Henrik Olsen, Magnus Löndahl
The Journal of Clinical Endocrinology & Metabolism.2023; 108(8): e536. CrossRef - Construction of a novel clinical nomogram to predict cancer-specific survival in patients with primary malignant adrenal tumors: a large population-based retrospective study
Mingzhen Li, Xiaoying Duan, Di You, Linlin Liu
Frontiers in Medicine.2023;[Epub] CrossRef - Primary Aldosteronism Prevalence – An Unfolding
Story
Suranut Charoensri, Adina F. Turcu
Experimental and Clinical Endocrinology & Diabetes.2023; 131(07/08): 394. CrossRef - Management of Adrenal Cortical Adenomas: Assessment of Bone Status in Patients with (Non-Functioning) Adrenal Incidentalomas
Alexandra-Ioana Trandafir, Mihaela Stanciu, Simona Elena Albu, Vasile Razvan Stoian, Irina Ciofu, Cristian Persu, Claudiu Nistor, Mara Carsote
Journal of Clinical Medicine.2023; 12(13): 4244. CrossRef - Clinical manifestations of functionally autonomous cortisol secretion in patients with adrenal masse
T. R. Chzhen, T. P. Kiseleva
Ural Medical Journal.2023; 22(3): 13. CrossRef - Tumor enlargement in adrenal incidentaloma is related to glaucoma: a new prognostic feature?
M. Caputo, T. Daffara, A. Ferrero, M. Romanisio, E. Monti, C. Mele, M. Zavattaro, S. Tricca, A. Siani, A. Clemente, C. Palumbo, S. De Cillà, A. Carriero, A. Volpe, P. Marzullo, G. Aimaretti, F. Prodam
Journal of Endocrinological Investigation.2023; 47(2): 377. CrossRef - Adrenal ganglioneuroma: Features and outcomes of cases series
Pei Li, Rongchang Zhang, Guang Wang, Jiongming Li
Asian Journal of Surgery.2023; 46(11): 5272. CrossRef - Recent Updates on the Management of Adrenal Incidentalomas
Seung Shin Park, Jung Hee Kim
Endocrinology and Metabolism.2023; 38(4): 373. CrossRef - Adrenal malakoplakia a rare lesion that mimics a neoplasm
Orión Erenhú Rodríguez González, Jesus Eduardo Osorio, Edgar Iván Bravo Castro
Urology Case Reports.2023; 51: 102568. CrossRef - LC-MS based simultaneous profiling of adrenal hormones of steroids, catecholamines, and metanephrines
Jongsung Noh, Chaelin Lee, Jung Hee Kim, Seung Woon Myung, Man Ho Choi
Journal of Lipid Research.2023; 64(11): 100453. CrossRef - Incidentaloma adrenal. Del hallazgo casual al diagnóstico definitivo
Mercedes Retamal Ortíz, Ana Belén Vicario Parada, Elena Vázquez Jarén
Actualización en Medicina de Familia.2023;[Epub] CrossRef - Diagnosis and management of adrenal incidentaloma: use of clinical judgment and evidence in dialog with the patient
Yusaku Yoshida, Kiyomi Horiuchi, Michio Otsuki, Takahiro Okamoto
Surgery Today.2023;[Epub] CrossRef - Can MDCT Enhancement Patterns Be Helpful in Differentiating Secretory from Non-Functional Adrenal Adenoma?
Svetlana Kocic, Vladimir Vukomanovic, Aleksandar Djukic, Jovica Saponjski, Dusan Saponjski, Vuk Aleksic, Vesna Ignjatovic, Katarina Vuleta Nedic, Vladan Markovic, Radisa Vojinovic
Medicina.2023; 60(1): 72. CrossRef - Computer-assisted Reporting and Decision Support Increases Compliance with Follow-up Imaging and Hormonal Screening of Adrenal Incidentalomas
Renata R. Almeida, Bernardo C. Bizzo, Ramandeep Singh, Katherine P. Andriole, Tarik K. Alkasab
Academic Radiology.2022; 29(2): 236. CrossRef - Incidental Adrenal Masses: Adherence to Guidelines and Methods to Improve Initial Follow-Up: A Systematic Review
Timothy Feeney, Andrea Madiedo, Philip E. Knapp, Avneesh Gupta, David McAneny, Frederick Thurston Drake
Journal of Surgical Research.2022; 269: 18. CrossRef - Incidental Adrenal Lesions May Not Always Require Further Imaging Work-up
Deborah A. Baumgarten
Radiology.2022; 302(1): 138. CrossRef - Adrenal Nodules Detected at Staging CT in Patients with Resectable Gastric Cancers Have a Low Incidence of Malignancy
Hae Young Kim, Won Chang, Yoon Jin Lee, Ji Hoon Park, Jungheum Cho, Hee Young Na, Hyungwoo Ahn, Sung Il Hwang, Hak Jong Lee, Young Hoon Kim, Kyoung Ho Lee
Radiology.2022; 302(1): 129. CrossRef - Management of incidental adrenal nodules: a survey of abdominal radiologists conducted by the Society of Abdominal Radiology Disease-Focused Panel on Adrenal Neoplasms
Michael T. Corwin, Nicola Schieda, Erick M. Remer, Elaine M. Caoili
Abdominal Radiology.2022; 47(4): 1360. CrossRef - Primary hyperaldosteronism: indications for screening
Novella M. Chikhladze
Terapevticheskii arkhiv.2022; 94(1): 107. CrossRef - Pathophysiological Link between Insulin Resistance and Adrenal Incidentalomas
Jordan A. Higgs, Alyssa P. Quinn, Kevin D. Seely, Zeke Richards, Shad P. Mortensen, Cody S. Crandall, Amanda E. Brooks
International Journal of Molecular Sciences.2022; 23(8): 4340. CrossRef - Can Radiomics Provide Additional Diagnostic Value for Identifying Adrenal Lipid-Poor Adenomas From Non-Adenomas on Unenhanced CT?
Binhao Zhang, Huangqi Zhang, Xin Li, Shengze Jin, Jiawen Yang, Wenting Pan, Xue Dong, Jin Chen, Wenbin Ji
Frontiers in Oncology.2022;[Epub] CrossRef - Adrenal Surgery in the Era of Multidisciplinary Endocrine Tumor
Boards
Costanza Chiapponi, Daniel Pinto Dos Santos, Milan Janis Michael Hartmann, Matthias Schmidt, Michael Faust, Roger Wahba, Christiane Josephine Bruns, Anne Maria Schultheis, Hakan Alakus
Hormone and Metabolic Research.2022; 54(05): 294. CrossRef - Optimal and novel imaging of the adrenal glands
Patrick J. Navin, Michael R. Moynagh
Current Opinion in Endocrinology, Diabetes & Obesity.2022; 29(3): 253. CrossRef - Adrenal Tumors in Young Adults: Case Reports and Literature Review
Małgorzata Zdrojewska, Emilia Mech-Siebieszuk, Renata Świątkowska-Stodulska, Bartosz Regent, Michał Kunc, Łukasz Zdrojewski, Krzysztof Sworczak
Medicina.2022; 58(6): 746. CrossRef - Incidence of malignancy in adrenal nodules detected on staging CTs of patients with potentially resectable colorectal cancer
Hae Young Kim, Yoon Jin Lee, Won Chang, Ji Hoon Park, Jungheum Cho, Hyeon Jeong Oh, Young Hoon Kim, Kyoung Ho Lee
European Radiology.2022; 32(12): 8560. CrossRef - Appendiceal Incidentalomas: Prevalence, Radiographic Characteristics, Management, and Outcomes
Adam Kelly, Stacy O’Connor, Diana Kane, Chiang-Ching Huang, Harveshp Mogal
Annals of Surgical Oncology.2022; 29(13): 8265. CrossRef - Laparoscopic large adrenal mass resection: why we should be more careful?
Mohsen Varyani, Mahmood Parvin, Hamidreza Akbari Gilani
African Journal of Urology.2022;[Epub] CrossRef - Serum Visfatin/NAMPT as a Potential Risk Predictor for Malignancy of Adrenal Tumors
Nadia Sawicka-Gutaj, Hanna Komarowska, Dawid Gruszczyński, Aleksandra Derwich, Anna Klimont, Marek Ruchała
Journal of Clinical Medicine.2022; 11(19): 5563. CrossRef - Application of radiomics in adrenal incidentaloma: a literature review
Cheng Li, Yan Fu, Xiaoping Yi, Xiao Guan, Longfei Liu, Bihong T. Chen
Discover Oncology.2022;[Epub] CrossRef - Hormone-inactive adrenal tumors in clinician’s practice
T. R. Chzhen, T. P. Kiseleva
Perm Medical Journal.2022; 39(5): 48. CrossRef - The diagnostic value of salivary cortisol and salivary cortisone in patients with suspected hypercortisolism
Vendela Berndt, Per Dahlqvist, Jennie de Verdier, Henrik Ryberg, Oskar Ragnarsson
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Role of Intraoperative Indocyanine Green (ICG) and Preoperative 3-Dimensional (3D) Reconstruction in Laparoscopic Adrenalectomy: A Propensity Score-matched Analysis
Giuseppe Palomba, Vincenza Paola Dinuzzi, Francesca Pegoraro, Roberto Ivan Troisi, Roberto Montalti, Giovanni Domenico De Palma, Giovanni Aprea
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2022; 32(6): 643. CrossRef - The Etiological Profile of Adrenal Incidentalomas
Fatima-Zahra Lahmamssi, Loubna Saadaoui, Hayat Aynaou, Houda Salhi, Hanan El Ouahabi
Cureus.2022;[Epub] CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - Conduite à tenir face à un fortuitome surrénalien chez le chien ou le chat
Diane Pichard, Ghita Benckekroun
Le Nouveau Praticien Vétérinaire canine & féline.2022; 19(82): 40. CrossRef - Laparoscopic transperitoneal adrenalectomy: a comparative study of different techniques for vessel sealing
Luca Cardinali, Edlira Skrami, Elisa Catani, Flavia Carle, Monica Ortenzi, Andrea Balla, Mario Guerrieri
Surgical Endoscopy.2021; 35(2): 673. CrossRef - Epidemiology and Comorbidity of Adrenal Cushing Syndrome: A Nationwide Cohort Study
Chang Ho Ahn, Jung Hee Kim, Man Young Park, Sang Wan Kim
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): e1362. CrossRef - Urine steroid profile as a new promising tool for the evaluation of adrenal tumors. Literature review
Marta Araujo-Castro, Pablo Valderrábano, Héctor F. Escobar-Morreale, Felicia A. Hanzu, Gregori Casals
Endocrine.2021; 72(1): 40. CrossRef - A Rare Neoplasm: Primary Adrenal Leiomyosarcoma
Jack T. Barnett, Christine W. Liaw, Reza Mehrazin
Urology.2021; 148: e11. CrossRef - Adrenal Ganglioneuroma Presenting as an Incidentaloma in an Adolescent Patient
Sonia G. Sharma, Steven N. Levine, Xin Gu
AACE Clinical Case Reports.2021; 7(1): 61. CrossRef - Feasibility of Iodine-131 6β-Methyl-Iodo-19 Norcholesterol (NP-59) Scintigraphy to Complement Adrenal Venous Sampling in Management of Primary Aldosteronism: A Case Series
Jeongmin Lee, Jeonghoon Ha, Sang-Kuon Lee, Hye Lim Park, Sung-Hoon Kim, Dong-Jun Lim, Jung Min Lee, Sang-Ah Chang, Moo Il Kang, Min-Hee Kim
International Journal of General Medicine.2021; Volume 14: 673. CrossRef - Best Achievements in Pituitary and Adrenal Diseases in 2020
Chang Ho Ahn, Jung Hee Kim
Endocrinology and Metabolism.2021; 36(1): 51. CrossRef - Adrenal surgery: Review of 35 years experience in a single centre
Enrico Battistella, Stefania Ferrari, Luca Pomba, Antonio Toniato
Surgical Oncology.2021; 37: 101554. CrossRef - Adrenocortical Carcinoma: A Case of Missed Diagnosis
Yusef Hazimeh, Carlie Sigel, Carsello Carie, Mathew Leinung, Zaynab Khalaf
Cureus.2021;[Epub] CrossRef - Imagerie fonctionnelle en endocrinologie : nouveaux paradigmes à l’horizon 2020
E. Marchal
Médecine Nucléaire.2021; 45(3): 158. CrossRef - Adrenal Incidentaloma
Caren G. Solomon, Electron Kebebew
New England Journal of Medicine.2021; 384(16): 1542. CrossRef - Can Hematological Parameters Play a Role in the Differential Diagnosis of Adrenal Tumors?
Mehmet Gürkan Arıkan, Göktan Altuğ Öz, Nur Gülce İşkan, Necdet Süt, İlkan Yüksel, Ersan Arda
Uro.2021; 1(2): 39. CrossRef - Incidental Adrenal Nodules
Daniel I. Glazer, Michael T. Corwin, William W. Mayo-Smith
Radiologic Clinics of North America.2021; 59(4): 591. CrossRef - Antioxidant Barrier and Oxidative Damage to Proteins, Lipids, and DNA/RNA in Adrenal Tumor Patients
Barbara Choromańska, Piotr Myśliwiec, Tomasz Kozłowski, Magdalena Łuba, Piotr Wojskowicz, Jacek Dadan, Hanna Myśliwiec, Katarzyna Choromańska, Anna Gibała, Anna Starzyńska, Małgorzata Żendzian-Piotrowska, Anna Zalewska, Mateusz Maciejczyk, Jos L. Quiles
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Laparoscopic Retroperitoneoscopic Removal of an Adrenal Hemangioma: a Case Report
Kristin McCoy, Katherine Howe, Daniel Tershak
Journal of Endocrine Surgery.2021; 21(3): 70. CrossRef - Metabolic Subtyping of Adrenal Tumors: Prospective Multi-Center Cohort Study in Korea
Eu Jeong Ku, Chaelin Lee, Jaeyoon Shim, Sihoon Lee, Kyoung-Ah Kim, Sang Wan Kim, Yumie Rhee, Hyo-Jeong Kim, Jung Soo Lim, Choon Hee Chung, Sung Wan Chun, Soon-Jib Yoo, Ohk-Hyun Ryu, Ho Chan Cho, A Ram Hong, Chang Ho Ahn, Jung Hee Kim, Man Ho Choi
Endocrinology and Metabolism.2021; 36(5): 1131. CrossRef - Cross-Talk Between Nitrosative Stress, Inflammation and Hypoxia-Inducible Factor in Patients with Adrenal Masses
Barbara Choromańska, Piotr Myśliwiec, Tomasz Kozłowski, Magdalena Łuba, Piotr Wojskowicz, Jacek Dadan, Hanna Myśliwiec, Katarzyna Choromańska, Katarzyna Makarewicz, Anna Zalewska, Mateusz Maciejczyk
Journal of Inflammation Research.2021; Volume 14: 6317. CrossRef - Cirugía laparoscópica en incidentaloma suprarrenal para el cirujano general: serie de casos
Martín Adrián Bolívar-Rodríguez, Marcel Antonio Cázarez-Aguilar, Pedro Alejandro Magaña-Zavala, Francisco Magaña-Olivas, José Martín Niebla-Moreno
Revista Mexicana de Cirugía Endoscópica.2021; 22(1): 8. CrossRef - Adrenal adenomas: what to do with them? Review 2
S. Rybakov
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(3): 241. CrossRef - Is Follow-up of Adrenal Incidentalomas Always Mandatory?
Giuseppe Reimondo, Alessandra Muller, Elisa Ingargiola, Soraya Puglisi, Massimo Terzolo
Endocrinology and Metabolism.2020; 35(1): 26. CrossRef - Imaging Findings of Primary Adrenal Leiomyosarcoma: A Case Report
Hye Ran Yoon, Dong Hee Park
Journal of the Korean Society of Radiology.2020; 81(2): 459. CrossRef - WFUMB position paper on the management incidental findings: adrenal incidentaloma
Christoph F. Dietrich, Jean Michel Correas, Yi Dong, Christian Nolsoe, Susan Campbell Westerway, Christian Jenssen
Ultrasonography.2020; 39(1): 11. CrossRef - A nationwide survey of adrenal incidentalomas in Japan: the first report of clinical and epidemiological features
Takamasa Ichijo, Hajime Ueshiba, Hajime Nawata, Toshihiko Yanase
Endocrine Journal.2020; 67(2): 141. CrossRef - Mimics, pitfalls, and misdiagnoses of adrenal masses on CT and MRI
Khaled M. Elsayes, Mohab M. Elmohr, Sanaz Javadi, Christine O. Menias, Erick M. Remer, Ajaykumar C. Morani, Akram M. Shaaban
Abdominal Radiology.2020; 45(4): 982. CrossRef - Adrenal Incidentaloma
Mark Sherlock, Andrew Scarsbrook, Afroze Abbas, Sheila Fraser, Padiporn Limumpornpetch, Rosemary Dineen, Paul M Stewart
Endocrine Reviews.2020; 41(6): 775. CrossRef - A Web Application for Adrenal Incidentaloma Identification, Tracking, and Management Using Machine Learning
Wasif Bala, Jackson Steinkamp, Timothy Feeney, Avneesh Gupta, Abhinav Sharma, Jake Kantrowitz, Nicholas Cordella, James Moses, Frederick Thurston Drake
Applied Clinical Informatics.2020; 11(04): 606. CrossRef - Presentation and outcome of patients with an adrenal mass: A retrospective observational study
Nadeema Rafiq, Tauseef Nabi, SajadAhmad Dar, Shahnawaz Rasool
Clinical Cancer Investigation Journal.2020; 9(5): 198. CrossRef - Evaluation of Functionality and Growth Rates in Adrenal Incidentalomas: Single Center Experience
Suna AVCI, Yüksel Aslı OZTURKMEN, Sayid ZUHUR, Gulkan OZKAN, Elif GUVEN, Nazan DEMİR, Yuksel ALTUNTAS
Phoenix Medical Journal.2020; 2(3): 125. CrossRef - Percutaneous Adrenal Radiofrequency Ablation: A Short Review for Endocrinologists
Byung Kwan Park
Endocrinology and Metabolism.2020; 35(4): 750. CrossRef - Autonomous cortisol secretion in adrenal incidentalomas
Marta Araujo-Castro, Miguel Antonio Sampedro Núñez, Mónica Marazuela
Endocrine.2019; 64(1): 1. CrossRef - Primary adrenal schwannoma: a series of 31 cases emphasizing their clinicopathologic features and favorable prognosis
Jun Zhou, Dandan Zhang, Wencai Li, Luting Zhou, Haimin Xu, Saifang Zheng, Chaofu Wang
Endocrine.2019; 65(3): 662. CrossRef - Challenging risk factors for right and left laparoscopic adrenalectomy: A single centre experience with 272 cases
Kadir Omur Gunseren, Mehmet Cagatay Cicek, Hakan Vuruskan, Yakup Kordan, Ismet Yavascaoglu
International braz j urol.2019; 45(4): 747. CrossRef - A case report on 111In chloride bone marrow scintigraphy in management of adrenal myelolipoma
Tatsuya Yamamoto, Mitsuru Koizumi, Atsushi Kohno, Noboru Numao, Kentaro Inamura
Medicine.2019; 98(8): e14625. CrossRef - PRACTICAL ASPECTS OF LAPAROSCOPIC ADRENALECTOMY IN CHILDREN WITH BENIGN ADRENAL TUMORS
I. V. Poddubny, R. S. Oganesyan, K. N. Tolstov, M. A. Kareva
Russian Journal of Pediatric Surgery.2019; 23(5): 248. CrossRef - Incidental neuroblastoma with bilateral retinoblastoma: what are the chances?
Kelsey Roelofs, Furqan Shaikh, William Astle, Brenda L. Gallie, Sameh E. Soliman
Ophthalmic Genetics.2018; 39(3): 410. CrossRef - Surgical Considerations in Subclinical Cushing’s Syndrome. When is it Time to Operate?
Alexander M. Nixon, C Aggeli, C Tserkezis, GN Zografos
Hellenic Journal of Surgery.2018; 90(1): 27. CrossRef - Adrenal incidentaloma – diagnostic and treating problem – own experience
Ryszard Pogorzelski, Krzysztof Celejewski, Sadegh Toutounchi, Ewa Krajewska, Tomasz Wołoszko, Małgorzata Szostek, Wawrzyniec Jakuczun, Patryk Fiszer, Małgorzata Legocka, Zbigniew Gałązka
Open Medicine.2018; 13(1): 281. CrossRef
- The improvement of postoperative blood pressure and associated factors in patients with hormone‐negative adrenal adenoma and hypertension

- A Case of an Adrenocortical Carcinoma with Pulmonary Embolism as the Initial Manifestation.
- Hyo Jin Lee, Ji Young Kwak, Young Jip Kim, Tae Ho Kim, Jan Dee Lee, Hyun Woo Lee, Hae Jin Kim, Dae Jung Kim, Yoon Sok Chung, Kwan Woo Lee, Seung Jin Han
- Endocrinol Metab. 2012;27(1):93-97. Published online March 1, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.1.93
- 1,962 View
- 26 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - The annual incidence of a first episode of deep vein thrombosis or pulmonary embolism (PE) in the general population is 120 per 100,000. Cancer is associated with an approximately 4- to 7-fold higher risk of thrombosis. Adrenocortical carcinoma (ACC) is a rare type of malignancy, accounting for 0.02% of all cancers reported annually. Approximately 40% of ACCs are nonsecretory. Most patients with nonsecreting tumors have clinical manifestations related to tumor growth (e.g., abdominal or flank pain). Often the adrenal mass is detected by chance via radiographic imaging. As a result, most ACC patients are diagnosed at an advanced stage and have a poor prognosis. Herein, we report a case of a 54-year-old woman who was admitted to our emergency department complaining of dyspnea. She was diagnosed with ACC accompanied by thrombi in the pulmonary artery and inferior vena cava. We performed a left adrenalectomy and administered adjuvant radiotherapy. The patient is currently receiving warfarin and adjuvant mitotane therapy. She was incidentally diagnosed with ACC, with PE as the initial manifestation.
-
Citations
Citations to this article as recorded by- Iliac vein deep vein thrombosis as an atypical presentation of an adrenocortical carcinoma
Arshpreet Singh Badesha, Taha Khan, Engy Abdellatif
BMJ Case Reports.2022; 15(5): e248708. CrossRef
- Iliac vein deep vein thrombosis as an atypical presentation of an adrenocortical carcinoma

- A Case of Persistent Hyperkalemia After Unilateral Adrenalectomy for Aldosterone-Producing Adenoma.
- Min Jae Yang, Seung Jin Han, Min Seok Lee, Eun Kyung Kim, Hae Jin Kim, Dae Jung Kim, Yoon Sok Chung, Tae Hee Lee, Jang Hee Kim, Kwan Woo Lee
- J Korean Endocr Soc. 2009;24(3):201-205. Published online September 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.3.201
- 1,871 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Primary aldosteronism is a syndrome characterized by various clinical features that are due to excessive autonomous aldosterone secretion not sustained by the activation of the renin-angiotensin system. Aldosterone-producing adrenal adenoma is found in approximately 35% of the patients who suffer with primary aldosteronism. Laparoscopic adrenalectomy is the standard treatment for aldosterone-producing adrenal adenoma, and the result of this operation is normalization of the serum potassium and plasma aldosterone concentrations, as well as correcting the plasma renin activity in most cases. However, it is known that some of the patients with aldosterone-producing adrenal adenoma show transient hyperkalemia postoperatively due to the reversible suppression of the renin-aldosterone axis. We recently experienced the case of a 54-year-old woman with an aldosterone-producing adrenal adenoma, and she presented with severe hyperkalemia after unilateral adrenalectomy. Compared with the previously reported cases that showed transient suppression of the rennin-aldosterone axis for less than 7 months, our patient revealed a prolonged episode of hyperkalemia for 8 months postoperatively, and this required continuous mineralocorticoid replacement.

- A Case Report of an Aldosterone-producing Adrenocortical Carcinoma.
- You Hong Lee, Tae Jin Park, Hae Jin Kim, Dae Jung Kim, Kwan Woo Lee, Myung Wook Kim, Jang Hee Kim, Tae Hi Lee, Yoon Sok Chung
- J Korean Endocr Soc. 2008;23(1):56-61. Published online February 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.1.56
- 1,794 View
- 27 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Primary aldosteronism is a syndrome characterized by hypokalemic alkalosis and hypertension. Aldosterone-producing adenomas and bilateral adrenal hyperplasia are common causes of this syndrome. An aldosterone-producing adrenocortical carcinoma is a very rare cause of primary aldosteronism. Recently we experienced a case of an aldosterone-producing adrenocortical carcinoma. A 41-year-old female was admitted for evaluation of a retroperitoneal mass. Because of hypokalemia and a history of hypertension, we evaluated the patient for primary aldosteronism. The high ratio of plasma aldosterone to renin activity suggested the possibility of the presence of primary aldosteronism. We performed adrenal vein sampling for differential diagnosis of an aldosterone-producing tumor from a retroperitoneal mass. The adrenal vein sampling showed that the primary aldosteronism was due to an aldosterone-producing tumor from the left adrenal gland. Surgical findings indicated that the retroperitoneal mass originated from the left adrenal gland and the pathological diagnosis for the mass was an adrenocortical carcinoma. In conclusion, the results from the adrenal vein sampling, as well as the surgical and pathological findings demonstrate that this case was an aldosterone-producing adrenocortical carcinoma.
-
Citations
Citations to this article as recorded by- Bone Mineral Density Reference of 10-20 year-old Korean Children and Adolescents - Based on Hologic DXA from the Korean National Health and Nutrition Examination Surveys -
Hyeon Jeong Lee, Bong sub Song, Dong Hwan Kim, Seung Youn Kim, Joong Bum Cho, Dong Ho Kim, Jun Ah Lee, Jung Sub Lim
Journal of Korean Society of Pediatric Endocrinology.2011; 16(2): 92. CrossRef
- Bone Mineral Density Reference of 10-20 year-old Korean Children and Adolescents - Based on Hologic DXA from the Korean National Health and Nutrition Examination Surveys -

- A Case Report of Symptomatic Salivary Gland Rest within the Pituitary Gland.
- Tae Ho Kim, Tae Jin Park, Hae Jin Kim, Dae Jung Kim, Yoon Sok Chung, Kwan Woo Lee, Tae Hi Lee, Ho Sung Kim, Kyung Gi Cho
- J Korean Endocr Soc. 2007;22(6):436-439. Published online December 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.6.436
- 1,796 View
- 22 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Although salivary gland tissues in the posterior pituitary are occasionally observed in microscopic examination at autopsy, these tissues are considered clinically silent. Only three examples of symptomatic salivary tissues in the pituitary have been previously reported. We report a case of symptomatic salivary gland rest within the pituitary gland. A 19-year-old woman complained of headache for 2 months, and dizziness, nausea, blurred vision for 1 week. Magnetic resonance imaging revealed a 1.8 cm-sized mass in sella turcica with hyperintensity on T1-weighted images. Basal hormone levels and combined pituitary stimulation test were normal. The trans-sphenoidal approach of tumor removal was performed and a pathological examination confirmed salivary gland rest without any evidence of a pituitary adenoma. The symptoms had disappeared, except for post-operative diabetes insipidus.
-
Citations
Citations to this article as recorded by- Symptomatic salivary gland choristoma of the pituitary gland
Pedro Iglesias, Cecilia Fernández-Mateos, Eva Tejerina
Endocrinología, Diabetes y Nutrición.2022; 69(7): 544. CrossRef - Symptomatic salivary gland choristoma of the pituitary gland
Pedro Iglesias, Cecilia Fernández-Mateos, Eva Tejerina
Endocrinología, Diabetes y Nutrición (English ed.).2022; 69(7): 544. CrossRef - Salivary gland tissues and derived primary and metastatic neoplasms: unusual pitfalls in the work-up of sellar lesions. A systematic review
T. Feola, F. Gianno, M. De Angelis, C. Colonnese, V. Esposito, F. Giangaspero, M.-L. Jaffrain-Rea
Journal of Endocrinological Investigation.2021; 44(10): 2103. CrossRef - Intrasellar Symptomatic Salivary Gland Rest with Inflammations
Yusuke Tanaka, Atsuhiko Kubo, Junichi Ayabe, Masahide Watanabe, Masahiro Maeda, Yukio Tsuura, Yoshihide Tanaka
World Neurosurgery.2015; 84(1): 189.e13. CrossRef - Intracranial Salivary Gland Choristoma within Optic Nerve Dural Sheath: Case Report and Review of the Literature
Eric B. Hintz, Gabrielle A. Yeaney, Glenn K. Buchberger, G. Edward Vates
World Neurosurgery.2014; 81(5-6): 842.e1. CrossRef
- Symptomatic salivary gland choristoma of the pituitary gland

- A Case of Resistance Syndrome to Thyroid Hormone Associated with Mutation (G345D) in the Thyroid Hormone Receptor Beta Gene.
- Tae Jin Park, Joon Koo Kang, Kyoung Woo Seo, Hae Jin Kim, Yoon Sok Chung, Kwan Woo Lee, Seon Yong Jeong, Hyon Ju Kim, Dae Jung Kim
- J Korean Endocr Soc. 2007;22(4):277-281. Published online August 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.4.277
- 1,953 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Resistance syndrome to thyroid hormone (RTH) is a rare autosomal dominant disease that is characterized by decreased tissue responsiveness to thyroid hormone, and it is mainly due to mutations of the thyroid hormone receptor beta (THRB) gene. We report here on a 36-years old male who had mild thyroid goiter and general weakness. The thyroid function test showed elevated levels of total T3 and free T4. The levels of TSH and the free alpha subunit were in normal ranges. Mutation analysis of the THRB gene revealed the missense mutation G345D. We report here on the clinical features and THRB gene mutation analysis of a case of RTH.
-
Citations
Citations to this article as recorded by- A Case of Resistance to Thyroid Hormone with Thyroid Cancer
Hee Kyung Kim, Doi Kim, Eun Hyung Yoo, Ji In Lee, Hye Won Jang, Alice Hyun Kyung Tan, Kyu Yeon Hur, Jae Hyeon Kim, Kwang-Won Kim, Jae Hoon Chung, Sun Wook Kim
Journal of Korean Medical Science.2010; 25(9): 1368. CrossRef
- A Case of Resistance to Thyroid Hormone with Thyroid Cancer

- A Case of Down's Syndrome with Thyrotoxic Crisis.
- Jae Ho Jung, Sang Mi Ahn, Hyon J Kim, Hae Jin Kim, Dae Jung Kim, Kwan Woo Lee, Yoon Sok Chung
- J Korean Endocr Soc. 2007;22(3):225-228. Published online June 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.3.225
- 1,650 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Patients with Down's syndrome have an increased prevalence of autoimmune disorders that affect both the endocrine and non-endocrine organs. The most common thyroid abnormality in Down's syndrome is subclinical hypothyroidism (12.5~32.5%). The occurrence of Down's syndrome in conjunction with hyperthyroidism is rare (0.6~2.5%). A 35-year old female was transferred to our hospital because of hypotension and mental change. She had suffered from a poor oral intake and general weakness for the previous 1 week. She had been admitted local hospital and was diagnosed as hyperthyroidism. On the third day after admission, she lost consciousness and was then transferred to University Hospital. Physical examination revealed hypotension (76/39 mmHg), sinus tachycardia (111/min) and tachypnea (28/min). The upward-outward slant of the palpebral fissures, epicanthal folds, low-set ears, short stature and clinodactyly were all identified. The thyroid gland was not enlarged and there was no evidence of ophthalmopathy. The serum free T4 concentration was 3.32 ng/dL, the T3 level was 212 ng/dL and the TSH level was 0.01 uIU/mL. She was positive for TBII. Abdominal computed tomography showed ascites and pneumoperitoneum. Primary closure was done on the duodenal ulcer perforation site. She was treated with transrectal propylthiouracil and intravenous esmolol. Chromosomal analysis revealed 47XX and 21 trisomy. She was finally diagnosed as Down's syndrome, Graves' disease and duodenal ulcer perforation. Her hyperthyroidism was controlled with PTU 100 mg after discharge.

- A Case of Familial Multiple Endocrine Neoplasia Type 1 with MEN1 Gene Mutation.
- Young Eun Jo, Yong Jun Choi, Yun Kyung Kim, Sang Mi Ahn, Sun Hye Jung, Hae Jin Kim, Dae Jung Kim, Kwan Woo Lee, Ji Hee Hong, Seon Yong Jeong, Hyon J Kim, Yoon Sok Chung
- J Korean Endocr Soc. 2007;22(1):68-73. Published online February 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.1.68
- 1,735 View
- 22 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Multiple endocrine neoplasia type 1 (MEN1) is an autosomal dominant disorder characterized by the combined occurrence of parathyroid, pancreatic islet and pituitary gland tumors. It is caused by mutation of the MEN1, a tumor suppressor gene, with more than 400 different MEN1 mutations having been described. Herein is reported the case of a 26-year-old woman who had complained of personality and behavior changes, coupled with repetitive loss of consciousness. Her random plasma glucose and insulin were 68 mg/dL and 67.3 microIU/mL, respectively. Two pancreatic masses were noted on abdominal computed tomography, with hypercalcemia noted from a routine chemistry test. Her diagnosis was that of MEN1; therefore, her first-degree relatives were also screened. DNA analysis was also performed, from which a MEN1 gene mutation (738del4 -> new nomenclature: 628del4) was detected. Knowledge of the MEN1 mutation status could provide early recognition of a tumor.
-
Citations
Citations to this article as recorded by- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1
Yoon Jung Chung, Sena Hwang, Jong Ju Jeong, Sun Yong Song, Se Hoon Kim, Yumie Rhee
Endocrinology and Metabolism.2014; 29(3): 270. CrossRef - Somatic Mutational Analysis of MEN1 and Phenotypic Correlation in Sporadic Parathyroid Tumors
Young Su Chae, Hee Jin Kim, Sun Wook Kim, Myung-Chul Chang
Journal of the Korean Surgical Society.2009; 76(1): 15. CrossRef
- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1

- Relationship between Diabetic Peripheral Vascular Disease and Ankle-Brachial Index.
- Bo Ram Koh, Yun Kyung Kim, Sang Mi Ahn, Kyoung Eun Song, Sun Hye Jung, Hae Jin Kim, Dae Jung Kim, Yoon Sok Chung, Kwan Woo Lee
- J Korean Endocr Soc. 2006;21(5):382-388. Published online October 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.5.382
- 1,911 View
- 20 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Peripheral vascular disease (PVD) is a primary risk factor of foot amputation. In patients with diabetes mellitus (DM), the frequency of PVD is twice that of the general population. The ankle-brachial index (ABI) is a valuable diagnostic test for PVD. In this study, we investigated the relationship between the ABI and PVD, as well as the cutoff value of ABI in the diagnosis of PVD, and analyzed whether the ABI can be used as a predictor for amputation. METHODS: Fifty-two type 2 DM patients (31 males, 21 females) underwent peripheral angiography. PVD was defined as the complete obstruction of arteries and/or significant luminal narrowing, with collateral vessels formation, using peripheral angiography. The ABI was calculated by measurement of the segmental pressure using the Doppler method. RESULTS: Significant differences were observed between PVD and non-PVD patients in terms of age, systolic pressure and total cholesterol (each P < 0.05). The ABI was significantly lower in legs with PVD (P < 0.01) and an ABI less than 0.90 was adequate for diagnosing PVD. The risk of amputation was significantly increased in relation to the ABI level, and the risk of amputation was 21.5 times greater in a leg with an ABI less than 0.40 compared to 0.90 (P = 0.021). CONCLUSION: ABI is a good diagnostic test for PVD and a good predictor of the need for amputation. -
Citations
Citations to this article as recorded by- The Relationship between Body Mass Index and Diabetic Foot Ulcer, Sensory, Blood Circulation of Foot on Type II Diabetes Mellitus Patients
Yi Kyu Park, Jun Young Lee, Sung Jung, Kang Hyeon Ryu
Journal of the Korean Orthopaedic Association.2018; 53(2): 136. CrossRef - The Relationship Between the Metabolic Syndrome and Systolic Inter-Arm Systolic Blood Pressure Difference in Korean Adults
Hyun Yoon, Seong Woo Choi, Jong Park, So Yeon Ryu, Mi Ah Han, Gwang Seok Kim, Sung Gil Kim, Hye Jong Oh, Cheol Won Choi
Metabolic Syndrome and Related Disorders.2015; 13(8): 329. CrossRef
- The Relationship between Body Mass Index and Diabetic Foot Ulcer, Sensory, Blood Circulation of Foot on Type II Diabetes Mellitus Patients

- The Relationship between the Leptin Concentration and the Small Dense Low Density Lipoprotein Cholesterol Concentration in Korean Type 2 Diabetic Patients.
- Wan Sub Shim, Hae Jin Kim, Eun Seok Kang, Yu Mie Rhee, Chul Woo Ahn, Sung Kil Lim, Hyun Chul Lee, Bong Soo Cha
- J Korean Endocr Soc. 2006;21(4):319-327. Published online August 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.4.319
- 1,838 View
- 20 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Leptin has been suggested as a possible cause of atherosclerotic disease. The small dense low-density lipoprotein cholesterol (LDL-C) has also been regarded as a new surrogate marker in atherosclerotic disease. The aim of this study was to evaluate the relationship between the leptin concentration and the small dense LDL-C concentration in Korean type 2 diabetic patients. METHODS: One hundred-ninety one type 2 diabetic patients, who did not use any medication that could affect the concentration of lipid such as statin, fibrate, thiazolidinediones and corticosteroid, were enrolled in this study. We analyzed the relationship between leptin, the small dense LDL-C and the other metabolic parameters. RESULTS: The small dense LDL-C concentrations were higher in the group with the highest tertile of the leptin value, both in males and females than those patients in the group with the lowest tertile of the leptin value. The small dense LDL-C concentrations were also higher in the group with the highest tertile of leptin divided by the BMI value both in males and females than those patients in the group with the lowest tertile of the leptin value. The leptin concentration was positively correlated with the small dense LDL-C, total cholesterol, triglyceride, LDL-C, insulin and HOMAIR values after adjusting for age, gender and BMI. CONCLUSION: The association between leptin and small dense LDL-C could be a factor that explains the association between leptin and cardiovascular disease. -
Citations
Citations to this article as recorded by- Relationships among Serum Adiponectin, Leptin and Vitamin D Concentrations and the Metabolic Syndrome in Farmers
Seo-Eun Yeon, Hee-Ryoung Son, Jung-Sook Choi, Eun-Kyung Kim
Korean Journal of Community Nutrition.2014; 19(1): 12. CrossRef - The Effect of Visceral Fat Area and Adipocytokines on Acute Myocardial Infarction: A Case-Control Study in Adult Korean Population
Kang-Kon Lee, Young-Sung Suh, Keun-Sang Yum
The Korean Journal of Obesity.2012; 21(1): 57. CrossRef
- Relationships among Serum Adiponectin, Leptin and Vitamin D Concentrations and the Metabolic Syndrome in Farmers

- Relationship between Childhood and Adolescent Obesity and Remnant Lipoprotein.
- Yong Jun Choi, Young Eun Jo, Yun Kyung Kim, Sang Mi Ahn, Seung Hee Baik, Sun Hye Jung, Hae Jin Kim, Yoon Sok Chung, Kwan Woo Lee, Dae Jung Kim
- J Korean Endocr Soc. 2006;21(4):311-318. Published online August 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.4.311
- 1,916 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Remnant lipoproteins are the lipolytic degradation product of the triglyceride-rich lipoproteins produced by the liver (very-low-density lipoprotein cholesterol) and intestine (chylomicrons). Recent studies have demonstrated a correlation between remnant lipoproteins and cardiovascular risk. Our study assessed the relationship between obesity and remnant lipoproteins and evaluated the factors related to remnant lipoprotein in children and adolescents. METHODS: Body mass index (BMI), waist circumference, systolic and diastolic blood pressures, body fat mass, total abdominal fat, visceral and subcutaneous fat areas, total cholesterol, triglyceride (TG), LDL cholesterol (LDL-C), HDL cholesterol (HDL-C) and remnant lipoprotein cholesterol (RLP-C) were measured in 135 children and adolescents (67 boys and 68 girls). Plasma RLP fractions were isolated using an immunoaffinity gel containing specific anti-apoB-100 and anti-apoA-I antibodies. The subjects were divided into three groups: the low (< 50 percentile), mid (50~84 percentile), and high (> or = 85 percentile) BMI groups. RESULTS: RLP-C was significantly correlated with age, sex, BMI, waist circumference, systolic and diastolic blood pressures, visceral and subcutaneous fat areas, visceral fat area to subcutaneous fat area ratio (VSR), total cholesterol, TG, HDL-C, apoB, and HOMA-IR. From a multivariate regression analysis, TG (beta = 0.928, P < 0.001) was found to be independently correlated with RLP-C. After excluding TG as an independent variable, a multivariate regression analysis revealed that the HOMA-IR (beta=0.231, P=0.007) and systolic blood pressure (beta=0.169, P=0.046) were independently associated with RLP-C. CONCLUSION: RLP-C was significantly higher in obese children and adolescents. TG, systolic blood pressure, and insulin resistance were related to remnant lipoproteins. -
Citations
Citations to this article as recorded by- Epidemiology of Childhood Obesity in Korea
Kyoung Hwa Ha, Dae Jung Kim
Endocrinology and Metabolism.2016; 31(4): 510. CrossRef
- Epidemiology of Childhood Obesity in Korea

- A Case of Metastatic Pulmonary Calcification in Primary Hyperparathyroidism.
- Kwang Eun Lee, Hae Jin Kim, Si Hoon Lee, Sang Woon Bae, Eun Seok Kang, Hae Won Chung, Hye Sun Seo, Dae Jung Kim, Sang Soo Chung, Sun Jung Kim, Young Duk Song, Sung Kil Lim
- J Korean Endocr Soc. 2002;17(4):583-588. Published online August 1, 2002
- 1,117 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - Metastatic calcification is the deposition of calcium, in previously normal tissue, as a result of elevated plasma calcium and phosphorus product levels and has been reported in patients with parathyroid adenoma, parathyroid carcinoma, hyperparathyroidism due to chronic renal failure, vitamin D intoxication, and osteolytic bone tumors, such as multiple myelomas. The lungs are the most common site of metastatic calcification. We have experienced metastatic pulmonary calcification in a case of primary hyperparathyroidism. A 55-year old woman was admitted due to general weakness. From the laboratory evaluation, hypercalcemia and excess production of parathyroid hormone (PTH) were noted. technetium-99m-labelled sestamibi scintigraphy indicated an intense uptake in the lower pole area of the left thyroid gland, suggestive of a parathyroid adenoma. A technetium-99m phosphate (99mTc-MDP) bone scan showed increased uptakes in both lungs. A parathyroid lobectomy was performed, and primary hyperparathyroidism, due to a parathyroid adenoma, was finally diagnosed. A follow-up 99mTc-MDP bone scan showed the disappearance of the metastatic pulmonary calcification, with the clinical symptoms and biochemical parameters normalizing after 6 months.


 KES
KES

 First
First Prev
Prev



